Sana Al-Yafaey1*, Nabil Al-Macki1
1Child health and Neurology Department, Royal Hospital, Ministry of Health, Oman
*Corresponding Author: Sana Al-Yafaey, M.Sc. Email: [email protected]
DOI: http://dx.doi.org/10.14206/canad.j.clin.nutr.2014.01.06
ABSTRACT
Epilepsy is a chronic non- communicable disorder of the brain that affects people of all ages in every country of the world. Among the different types of treatment options for epileptic patients, anti- epileptic drugs (AEDs) are the first line treatment by decreasing seizures. Nevertheless, different antiepileptic drugs can have different side effects. The most common side effects include; learning and attention problems, changes in mood or behavior, vitamin D serum reduction and interferes with the metabolism of calcium. The negative effects of antiepileptic drugs on the bone metabolism are one of the most significant and discussed side effects. Therefore, the present review aimed to discuss non-pharmacological approaches for management of epilepsy.
Full Text
INTRODUCTION
Epilepsy is a medical condition that produces seizures affecting a variety of mental and physical functions. It is also called a seizure disorder. When a person has two or more unprovoked seizures, they are considered to have epilepsy (1). A seizure is a sudden surge of electrical activity in the brain that usually affects how a person feels or acts for a short time. Seizures are not a disease in themselves. Instead, they are a symptom of many different disorders that can affect the brain. Some seizures can hardly be noticed, while others are totally disabling (2). Epilepsy in those with a genetic cause is normally referred to as, idiopathic epilepsy) (1, 2). There is a link between family history and consanguineous marriages, where it was reported that the familial clustering of epilepsy was higher in first degree compared to second degree relatives (3). Moreover, a case control study done in United Arab of Emirates showed that family history and consanguinity had an association with epilepsy (4).
Idiopathic epilepsy without mental retardation or any disabilities has various negative effects on the patient’s social life especially married life (5, 6). A recent study documented that consanguinity in parents of the epilepsy patients was significantly higher when compared to the general population (7). In approximately 60 per cent of cases, the cause of epilepsy is not known, and is referred to as cryptogenic epilepsy (8). There are also secondary causes to epilepsy such as brain damage, as a result of injury, deprivation of oxygen at birth, infections such as encephalitis or meningitis, malformation or degeneration of the brain and brain tumors (9). Metabolic causes include hypoglycemia, calcium, drugs and alcohol consumption (10).
Epilepsy’s Prevalence and Incidence
World Health Organization (WHO) estimated that, on 2012 around 50 million people worldwide have epilepsy with nearly 80% found in developing regions (11). In children of age 0-15, epilepsy is considered to be the most common neurological disorders with an incidence of 5-7 per 10000 yearly (12). A Scandinavian study showed that epilepsy prevalence rates among school children varied from 2.4-11.6 per 1000 children (13).Approximately 724,500 people with epilepsy live in the Arab world, and the prevalence ranged between 0.9/1000 in Sudan and 6.5/1000 in Saudi Arabia, with a median of 2.3/1000 (14).
Types of Seizures
As illustrated on figure 1, seizures are grouped into two main categories: generalized seizures and focal (partial) seizures. Generalized seizures: This type of seizure, the whole brain is affected by changed electrical activity and the child becomes unconscious of their surroundings, and the following are some examples of generalized seizures: Tonic-clonic seizures, Tonic seizures, Atonic seizures, Myoclonic seizures and Absence seizures (15).
Focal (partial) seizures: Focal refers to the seizure coming from one area of the brain, and the following are types of focal seizures: Temporal lobe epilepsy, Frontal lobe epilepsy, Occipital lobe epilepsy and Parietal lobe epilepsy (10).
Management of Epilepsy
Antiepileptic drugs (AEDs) are considered the first line treatment option for epileptic patients. In addition, promising results have been reported while using the alternative methods for treatment such as ketogeinc diet, vagus nerve stimulation, and surgery, complementary and alternative medicine.
1. Ketogeinc Diet
The ketogenic diet is a high-fat, low-carbohydrate and adequate -protein diet, which may be considered for children who failed to respond with at least two antiepileptic medications. Up to date the information about how the diet exactly helps in reducing seizures is not quite known but, many believe that as there is almost no enough amounts of carbohydrates , the body starts breaking down the fat to provide energy and this process produces metabolites called ketones. The ketone bodies will be the main source of energy to the brain. The production of ketone bodies is thought to alleviate seizures. The common ratios of fats to carbohydrates and protein by grams are 3:1 or 4:1 (16). It is important to know that while using the ketogenicdiet; a few of parameters are followed, similar to using medication, such as: the patient’s seizure control and lack of side effects, adequate growth. Adherence to the regimen can be followed with a simple laboratory measurement that can be done at home, ketonuria. Ketonuria (specifically, β-hydroxybutyrate and acetoacetate) is the most common way to measure adherence to the ketogenic diet regimen it is an easy and relatively cost-effective indicator of ketosis (17).The efficacy of the ketogenic diet was reported to be high in early studies, with 60% of patients enjoying total freedom from seizures, and another 35% showing greater than 50% decrease in seizure frequency.
A retrospective analysis of the Hopkins cohort prior tothe most recent resurgence of interest in the diet showed that 29% of patients had nearly complete control of their seizures (18). This kind of diet should be done only under the supervision of a well-trained dietitian and a neurologist. Some of the side effects that can be developed when starting this kind of diet are poor development; the diet is also inadequate in trace elements, minerals and certain vitamins (19). Therefore, supplementation is necessary in order to avoid nutritional deficiencies, including Ca, Zn, folic acid, Se, Fe and vitamin D (20, 21). Other effects are predictable, preventable, and potentially treatable, such as dehydration and hypoglycemia (22).
Another type of ketogenic diet beside the classical method of the diet is to adopt a diet rich in medium-chain triacylglycerols (MCT) rich diet, it provides 60% of MCT, 11% of long chain saturated fats, 10% of protein and19% of carbohydrates (23). The MCT diet has greater adverse effects, but can be as effective as the classic ketogeinc diet method in controlling epileptic seizures (24, 25). A retrospective study using the classical and MCT diet, assessed seizure control based on the percentage change of patients’ seizure frequency, the results indicated that only seven patients out of 52 remained on the diet for more than 1 year and while on the diet, a greater than 50%decrease in seizure frequency happened in thirty-five patients (67·3 %) of whom six (11·5 %) were seizure-free (26). Another study included 143 patients (mean age 7·5 years) indicated that patients with generalized seizures responded better to the diet than patients with focal seizures, but the difference between the groups was not significant, and approximately 25% of those with focal seizures had 50% improvement in seizure activity after 3 months and have greater than 90% improvement (27).
It is suggested that, regardless of the seizure type, the ketogeinc diet is an effective treatment and represents a potential therapeutic option if surgery is not possible. Other types of diets believed to be for treating epilepsy is the modified Atkins diet which has been found to be effective and well tolerated (16).
2. Vagus Nerve Stimulation
This treatment consists of a computerized electrical device that stimulates the vagus nerve at preset intervals and intensities of current, such impulses on the vagus nerve desynchronized seizure activity in the brain (28, 29).
3. Surgery
The most common types of surgeries include; Lesion ectomy (which is the removal of a lesion or area of injury or damage to the tissue structure), Focal resection (removal of the area of the origin of seizures), Lobectomy (removal of a lobe of the brain), Hemispherectomy (used to treat severe epilepsy in children) (30). About 50% of patients who undergo surgery will be totally seizure-free and another 25% have only 1-2 seizures per year after surgery (10, 11).
4. Complementary and Alternative Medicine
A systematic review aimed to estimate the prevalence of use of complementary and alternative medicine (CAM) in the UK found that across surveys on CAM in general, the average one-year prevalence of use of CAM was 41.1% and the average lifetime prevalence was 51.8%. In methodologically sound surveys, the equivalent rates were 26.3% and 44%, respectively. In surveys with response rates >70%, average one-year prevalence was nearly threefold lower than in surveys with response rates between 21% and 50%. Herbal medicine was the most popular CAM, followed by homeopathy, aromatherapy, massage and reflexology (31). Moreover, another study done to assess the usage and perceptions of CAM by patients with epilepsy in the Midwest of the United States, among adult patients with epilepsy, and data were collected from 228 patients. It was reported that Thirty-nine percent reported using CAM; 25% reported using CAM specifically for their epilepsy. Prayer/spirituality was the most commonly used form of CAM (46%); followed by “mega” vitamins (25%), chiropractic care (24%), and stress management (16%) (32).
CONCLUSION
This review highlighted the importance of adopting non-pharmacological approaches for epilepsy management and treatment to overcome the antiepileptic drugs-mediated side effects including impairment of calcium homeostasis and liver toxicity.
REFERENCES
- Chang BS, Lowenstein DH. Epilepsy. New Eng J Med 2003; 349 (13): 1257–1266.
- Fisher R, van Emde, Boas W, Blume W, Elger C, Genton P, et al. Epileptic seizures and epilepsy: definitions proposed by the International League against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 2005; 46 (4): 470-472.
- Ottman R, Lee JH, Risch N, Hauser WA, Susser M. Clinical indicators of genetic susceptibility to epilepsy. Epilepsia 1996; 37:353-361.
- Khan H, Mohamed A, Al-Sakini Z, Zulfiquar K, Sohail A, Shaikh, et al. Consanguinity, family history, and risk of epilepsy: a case control study. Gulf Med J 2012; 1(1):32-36.
- Wada K, Kawata Y, Murakami T, Kamata A, Zhu G, Mizuno K, et al. Sociomedical aspects of epileptic patients: their employment and marital status. Psych Clin Neurosci 2001; 19:141-146.
- Ramasundrum V, Tan CT. Consanguinity and risk of epilepsy. Neuro Asia 2004; 9 (1): 10-14.
- Mehndiratta MM, Paul B, Mehndiratta P. Arranged marriage, consanguinity and epilepsy. Neuro Asia 2007; 12:15-17.
- Epilepsy Research UK. What Is Epilepsy? http://www.epilepsyresearch.org.uk/ (Accessed on December 2013).
- Berg AT, Scheffer IE. New concepts in classification of the epilepsies: entering the 21stcentury. Epilepsia 2011; 52(6): 1058-1062.
- Solomon N, Mchale K. An overview of epilepsy in children and young people. Learning Disability Practice 2012; 15 (6):30-38.
- WHO Fact Sheet—Epilepsy: Epidemiology, Etiology and Prognosis. Available from URL: http://www.who.int/mediacentre/factsheets/fs999/en/index.html (accessed on December 2013).
- Cansu A. Antiepileptic drugs and hormones in children. Epilep Res 2010; 89: 89-95.
- Sidenvall R, Forsgren L, Heijbel J. Prevalence and characteristics of epilepsy in children in Northern Sweden. Seizure 1996; 5:139- 146.
- Benamer HT, Grosset DG. A systematic review of the epidemiology of epilepsy in Arab countries. Epilepsia 2009; 50(10):2301–2304.
- Park JH, Jung IA, Han JY, Sung IK, Lee JY, Youn YA, et al. Neonatal Seizures in Preterm in infants. J Korean Child Neurology Society 2012; 20(3):188-195.
- Kossoff EH, McGrogan JR. Worldwide use of the ketogenic diet. Epilepsia 2005; 46:280–289.
- Hartman AL, Vining EP. Clinical aspects of the ketogenic diet. Epilepsia 2007; 48(1):31–42.
- Kinsman SL, Vining EP, Quaskey SA, Mellits D, Freeman JM. Efficacy of the ketogenic diet for intractable seizure disorders: review of 58 cases. Epilepsia 1992; 33:1132–1136.
- DiMario FJ, Holland J. The ketogenic diet: a review of the experience at Connecticut Children’s medical center. Pediatric Neurology 2002; 26: 288–292.
- Thiel RJ, Fowkes SW. Down syndrome and epilepsy: a nutritional connection? Medical Hypotheses 2004; 62; 35- 44.
- Hossain SA, La Vega-Talbott M, Solomon GE. Ketogenic diet in pediatric epilepsy patients with gastrostomy feeding. Pediatric Neurology 2005; 32: 81–83.
- Kang HC, Chung DE, Kim DW, Kim HD. Early- and late-onset complications of the ketogenic diet for intractable epilepsy. Epilepsia 2004; 45:1116–1123.
- Thavendiranathan P, Mendonca A, Dell C, Likhodii SS, Musa K, Iracleous C, et al. The MCT ketogenic diet: effects on animal seizure models. Experimental Neurology 2000; 161: 696–703.
- Liu MC, Williams S, Hammond C, Stephens D, Curtis R. A prospective study: growth and nutritional status of children treated with the KD. J Am Diet Asso 2003; 103:707–712.
- Edelstein SF, Chisholm M. Management of intractable childhood seizures using the non-MCT oil ketogenic diet in 20 patients. J Am Diet Asso 1996; 96:1181–1182.
- Hassan AM, Keene DL, Whiting SE, Jacob PJ, Champagne JR, Humphreys P. Ketogenic diet in the treatment of refractory epilepsy in childhood. Pediatric Neurology 1999; 21:548–552.
- Maydell BV, Wyllie E, Akhtar N, Kotagal P, Powaski K, Cook K, et al. Efficacy of the ketogenic diet in focal versus generalized seizures. Pediatric Neurology 2001; 25:208–212.
- Kotagal P. Neurostimulation: vagus nerve stimulation and beyond. Seminars in Pediatric. Neurology 2011;18(3):186-194.
- Koul R. Non-convulsive status epileptics in children, a report of 12 cases. Neurosciences 2000; 5 (1): 13-17.
- Cross JH. Epilepsy surgery in childhood. Epilepsia 2002; 43(3): 65-70.
- Posadzki P, Watson LK, AlotaibiA, Ernst E. Prevalence of use of complementary and alternative medicine (CAM) by patients/consumers in the UK: systematic review of surveys. Clinic Med 2013; 13(2):126-131.
- Liowa K, Ablahb E, Nguyenb JC, Sadlera T, Wolfeb D, et al. Pattern and frequency of use of complementary and alternative medicine among patients with epilepsy in the Midwestern United States. Epilep Behav 2007; 10(4):576-582.
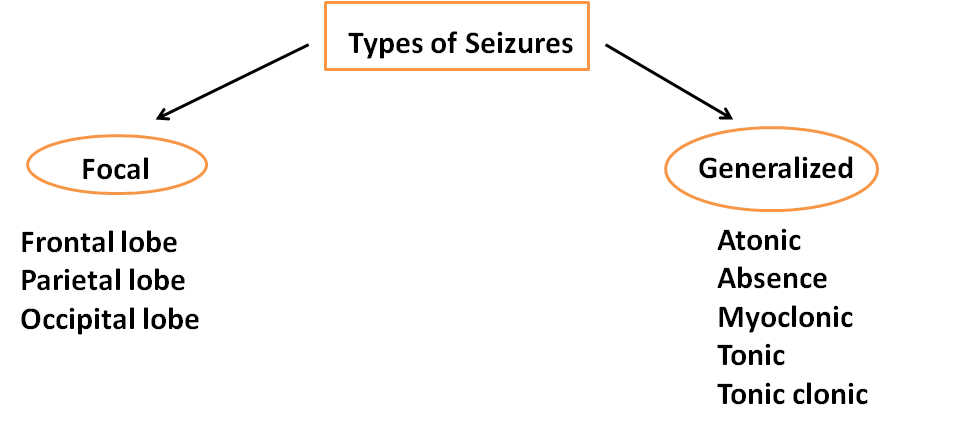
Figure 1: Electrical Activity Areas in Focal and Generalized Seizures
